Experienced physicians in specialized AD centers can now diagnose AD with up to 90 percent accuracy. Early diagnosis has advantages:
- Doctors can rule out other conditions that may cause dementia.
- If it is AD, families have more time to plan for the future.
- Treatments can start earlier, when they may be more effective.
- It helps scientists learn more about the causes and development of AD.
Comprehensive Workup for Diagnosis of Alzheimer’s disease
One of the main goals in diagnosing Alzheimer’s disease is to make it as early as possible. The introduction of techniques such as imaging are assisting doctors in making a rather accurate diagnosis of probable Alzheimer’s disease.
Diagnosing Alzheimer’s requires careful medical and neurological evaluations, including:
- Medical History & Physical Examination
- Laboratory tests
- Neuropsychological
- Brain Imaging scans
1. Medical History and Physical Examination
This is to gain information about the person’s health history including present and past medical conditions, use of prescription drugs and lifestyle. Vision, hearing and blood pressure will also be examined. Neurological tests will be conducted to evaluate reflexes ,coordination and eye movement. Questions will be asked to the person about his/her ability to carry out daily activities, any changes in personality or behavior. A family member or caregiver may be asked to comment on the person’s mental function and the duration of symptoms such as memory loss, change in behavior and personality.
2. Laboratory tests
It is important to recognize that conditions other than Alzheimer’s disease can provoke confused thinking, trouble focusing or even memory loss. Such conditions include anemia, depression, infection, diabetes, kidney disease, liver dysfunction ,thyroid abnormalities and cardiovascular and respiratory problems. By performing blood and urine tests these conditions can be established or ruled out. For instance hypothyroidism or failure to produce sufficient thyroid hormones, which is common in the elderly and can cause dementia. Dementia may also be the result of a vitamin B12 deficiency, a condition common in older people. It is recognized that 15 % of dementias are reversible.
3. Neuropsychological Tests
These tests are aimed to determine the degree of difficulties in attention, perception, memory, language, problem solving, and social skills. Depression and mood can also be evaluated with these tests. Common tests used are the following:
- MMSE (Mini Mental Status Examination)
- CDR (Clinical dementia rating)
- Clock Drawing Test
- SIB (Severe Impairment Battery)
- ADCS-ADL (Alzheimer’s disease cooperative study activities of daily living
- BGP (Behavioral rating scale for geriatric patients)
- FAST (Functional Assessment Staging)
- NPI (Neuropsychiatric inventory)
- CIBIC-Plus (Clinicians interview-based impression of change plus caregiver input)
Mini-Mental Status Examination (MMSE) is one of the most common tests and is used to:
- Assess cognitive mental status as an initial evaluation tool or evaluation of treatment
- Assess orientation, attention, immediate and short-term recall, language, and the ability to follow simple verbal and written commands
4. Neuroradioimaging Brain Scans
- Computed tomography CT First –line examination to rule out causes of surgical and thus reversible ,dementia such as subdural hematoma or normal pressure hydrocephalus
- Magnetic resonance imaging MRI- Magnetic resonance-based volume measurements of atrophy are potential markers of the progression of Alzheimer’s disease, starting from the preclinical stages.
- Positron-emission testing PET- Imaging with [18F]-2-fluoro-2deoxy-D-glucose (FDG) is accurate for early diagnosis.
- MRI preferred over CT
- Assess degree of Medial Temporal Lobe Atrophy
- Amygdala, Hippocampus, Parahippocampal gyrus
- Rule out other causes dementia
EXCITING NEW DEVELOPMENTS IN DIAGNOSTICS
Amyloid Imaging
- Science Daily (Mar. 28, 2008) — A groundbreaking study conducted by University of Pittsburgh Alzheimer’s disease researchers reported in the journal Brain confirms that Pittsburgh Compound-B (PiB) binds to the telltale beta-amyloid deposits found in the brains of patients with Alzheimer’s disease. The finding is a significant step toward enabling clinicians to provide a definitive diagnosis of Alzheimer’s disease in living patients. Until now, the beta-amyloid deposits to which PiB binds have been confirmed, without question, only in the autopsied brains of patients afflicted with Alzheimer’s.
- The new findings, which correlate PiB-identified beta-amyloid deposits from living patients to their post-mortem autopsy results, will ultimately aid in the early diagnosis of Alzheimer’s, help clinicians monitor the progression of the disease and further the development of potential treatments.
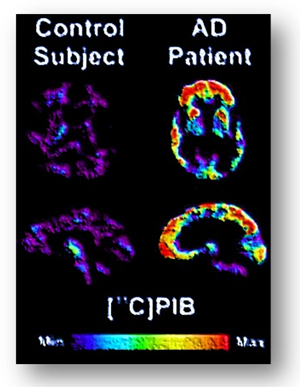
Brain PET scan using [C14] PiB showing dramatic amyloid plaque deposition in the AD patient (right) but not in the healthy control subject (left).
*Image courtesy of the National Institute on Aging/National Institutes of Health*
GUIDELINES FOR DIAGNOSIS OF ALZHEIMER’S DISEASE
Since Alzheimer’s disease is a type of the many dementias how is this disorder differentiated from other dementias? Clinicians use specific criteria to establish a diagnosis of Alzheimer disease.
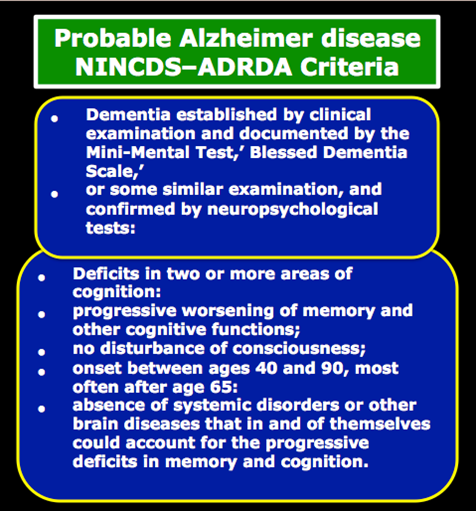
The two most commonly used criteria for the diagnosis of AD are those of created by the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) joint task force in 1984 (McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 1984;34:939-944) and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)
NINCDS-ADRDA criteria
In 1984, a task force established by the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) put forth a set of clinical criteria for the diagnosis of PROBABLE, POSSIBLE, and DEFINITE Alzheimer’s disease. These criteria link clinical patterns to neuropathology. It should be noted that a definitive diagnosis of Alzheimer’s disease is only made post-mortem, where autopsy can reveal the presence of beta-amyloid plaques and neurofibrillary tangles. Symptoms of Alzheimer’s-type dementia include a gradual loss of memory and cognitive disturbances that cause significant impairment.
The original NINCDs-ADRDA criteria have received updates and undergone revisions, and have been incorporated into major international criteria, including the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases
DSM IV criteria
The other commonly used clinical criteria for AD diagnosis are derived from the current version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) pub- lished by the American Psychiatric Association.(American Psychiatric Association. Diagnostic and statistical manual of mental disorders (IV-TR). 4th ed (revised). Washington, DC 2000)
A. The development of multiple cognitive deficits manifested by both
A1. MEMORY impairment (impaired ability to learn new information or to recall previously learned information)
A2. ONE or MORE of the following cognitive disturbances:
-
-
- Aphasia — a deterioration of language abilities, which can manifest in several ways
- Apraxia — difficulty executing motor activities, even though movement, senses, and the ability to understand what is being asked are still intact
- Agnosia — an impaired ability to recognize or identify objects, even though sensory abilities are intact
- Problems with executive functioning, such as planning tasks, organizing projects, or carrying out goals in the proper sequence
-
B. The cognitive deficits in Criteria A1 and A2 each cause significant impairment in social or occupational functioning and represent a significant decline from a previous level of functioning.
C. The course is characterized by gradual onset and continuing cognitive decline.
D. The cognitive deficits in Criteria A1 and A2 are not due to any of the following:
- other central nervous system conditions that cause progressive deficits in memory and cognition (e.g., cerebrovascular disease, Parkinson’s disease, Huntington’s disease, subdural hematoma, normal-pressure hydrocephalus, brain tumor)
- systemic conditions that are known to cause dementia (e.g., hypothyroidism, vitamin B or folic acid deficiency, niacin deficiency, hypercalcemia, neurosyphilis, HIV infection)
- substance-induced conditions
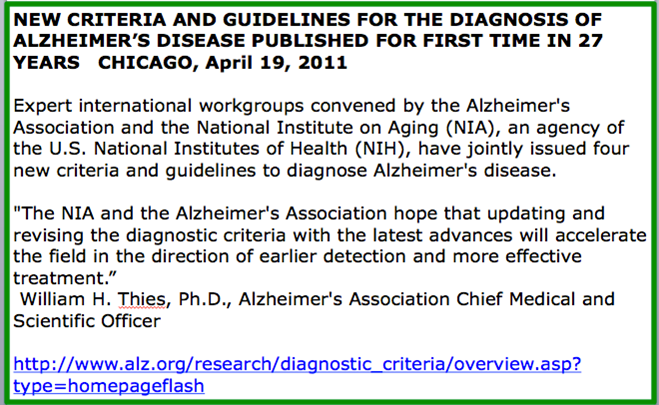
DIAGNOSING ALZHEIMER’S DISEASE: 2011 and beyond
The criteria to diagnose Alzheimer’s disease established by NINCDS-ADRDA remained rock solid for 25 years. However in 2009 there was an overwhelming consensus that the diagnosis of AD needed to be revised to take into account the scientific advances in the field. The National Institute on Aging (NIA) and the Alzheimer’s Association sponsored a series of advisory round table meetings in 2009 whose purpose was to establish a process for revising diagnostic and research criteria for the continuum of AD. In 2011, new criteria and guidelines that update, refine, and broaden the ones published in 1984 were issued. For further reading about these new guidelines please go to the following link.